Step One: Understanding the Social Determinants of Health
How Social Factors Impact Patient Health & Outcomes
Before implementing SDOH screening and other best practices, clinicians need a basic understanding of the social determinants of health
Research on the social determinants of health continues to evolve at a rapid pace. Healthcare organizations, higher education institutions, government agencies, and non-profits have invested a variety of resources to better understand and communicate the importance of SDOH, especially in terms of how it relates to medical care.
What Are Social Determinants of Health?
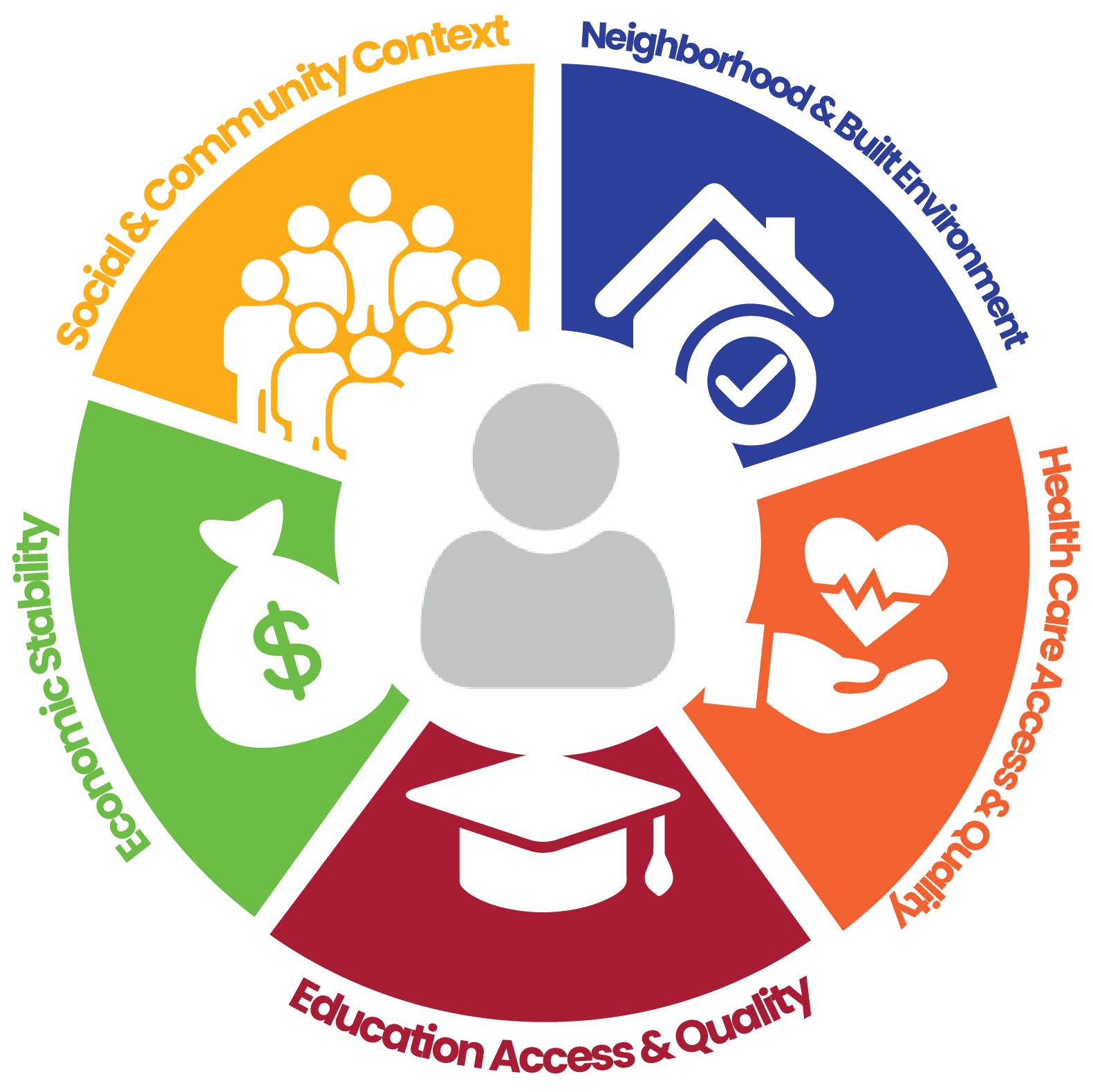
Social determinants of health are the non-medical factors that influence health outcomes. They include characteristics of the environments where we grow, live, learn, work, play, worship, and age. The conditions in these environments shape our health, well-being, and quality of life.
It is widely accepted that SDOH is comprised of five main categories:
- Education Access & Quality: Graduation rates, language & literacy, and early childhood education & development
- Neighborhood & Built Environment: Housing quality, access to transportation, and community violence & crime
- Social & Community Context: Supportive community, workplace conditions, incarceration, and racism
- Economic Stability: Poverty, employment, food security, and housing stability
- Healthcare Access & Quality: Health literacy, insurance coverage, and access to healthcare
SDOH’s Relationship to Health Disparities & Inequities

What do SDOH barriers look like in reality?
Consider an individual living in a rural Arizona community. The community’s main source of groceries is the local dollar store, which does not stock a wide variety of fresh foods such as fruits and vegetables.
Due to the community’s lack of access to nutritious food, the population is less likely to maintain a healthy diet, even when encouraged by their physicians.
In turn, this increases their risk of developing conditions such as heart disease, diabetes, and obesity, which potentially shortens their life expectancy compared to those in the neighboring town, who have access to healthier food options.
As the case study illustrates, merely promoting healthy choices is not enough to eliminate health disparities and inequities. Instead, public health organizations, along with their partners in sectors like education, transportation, and housing, must take proactive steps to enhance the conditions in people’s environments.
Exploring the Different Social Determinants of Health
Within the five main categories of social determinants of health, there are a broad number of contributing factors, including access to key resources, social supports, and physical safety. Learn more about these factors below.
Start Step Two of Implementing SDOH Screening:
With a working knowledge of SDOH under your belt, you’re ready to explore methods of preparing your practice for screening.
Continue Your SDOH Learning
ArMA’s SDOH Center of Excellence offers physicians many opportunities to continue their learning and exploration of the non-medical factors impacting patients. For more resources, including webinars, whitepapers, and more, visit our Resources webpage.